Reperfusion injury: Why restoring blood flow can still cause harm
Reperfusion saves lives — but it can also hurt. When blood returns to tissue after a period of low flow, a sudden spike of oxygen and immune activity can damage cells. Reperfusion injury shows up after heart attacks, strokes, limb surgery, and organ transplants. Recognizing the problem and using proven strategies reduces long-term harm.
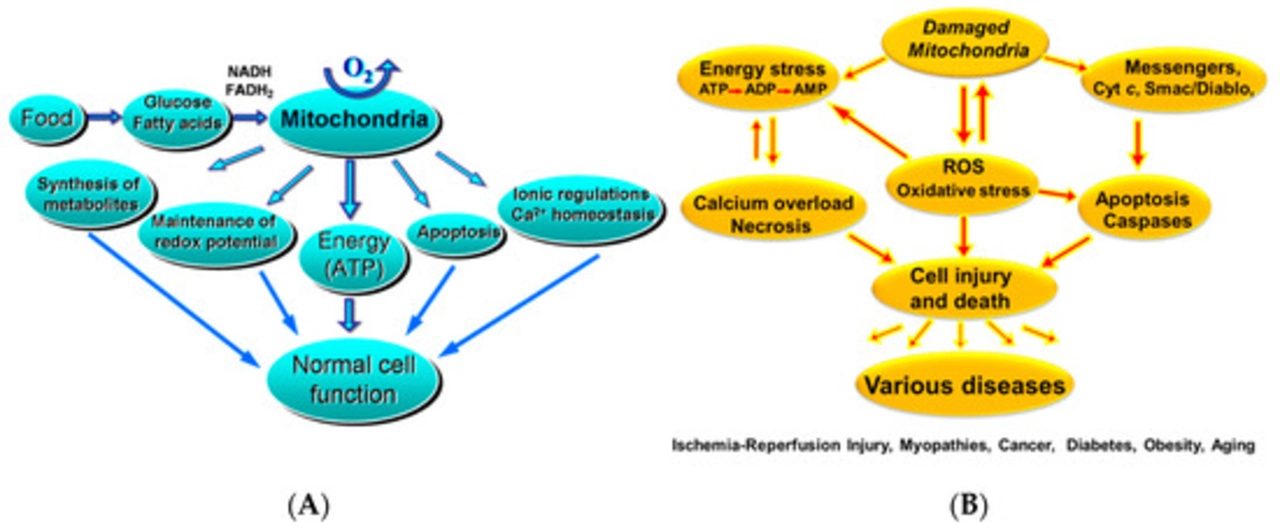
The core of the damage is predictable. Oxygen produces free radicals that damage membranes. Cells let in too much calcium and swell. The immune system floods the area and ramps up inflammation. All together this can worsen tissue death, cause arrhythmias in the heart, increase swelling in the brain, or make grafts fail.
Clinically, reperfusion issues look different by organ. After a heart attack you may see chest pain, abnormal heartbeats, or a rise in cardiac enzymes despite opening the artery. After stroke, swelling and worsening neurological deficits can appear hours after flow is restored. In transplanted organs early dysfunction, pink or mottled tissue, or fast rising markers of damage suggest reperfusion injury.
How teams reduce risk
What helps? A mix of timing, technique, and medication. For teams treating heart attacks, faster but controlled opening of the artery matters. Doctors use techniques like gradual reperfusion, filter devices, and careful blood pressure control. In surgery, cooling the organ or tissues before reperfusion lowers metabolic demand. Remote ischemic conditioning — brief cycles of blood flow restriction on an arm or leg before reperfusion — is an easy, low-risk trick that shows promise.
Medications that lower oxidative stress and inflammation can reduce injury. Antioxidants like N-acetylcysteine, certain statins, and targeted anti-inflammatory drugs have been tested with mixed results. Some centers use cyclosporine or similar agents around reperfusion for heart attacks, though benefits remain under study. No single drug fixes the problem; combining strategies usually works better.
Ongoing research and what it means for you
Research keeps evolving. Trials are testing new antioxidants, cell therapy, and drugs that stabilize mitochondria — the cell’s energy units. If you follow medical news, look for studies that report clear clinical outcomes, not just laboratory markers. Animal studies are useful, but human results matter most.
For patients, the practical steps are simple. If you or a loved one needs an urgent procedure for a blocked artery or a transplant, ask the team how they manage reperfusion risk. Ask about timing, temperature control, and whether they use protective techniques like postconditioning or remote conditioning. After the procedure, report new or worsening pain, sudden shortness of breath, palpitations, or increased confusion right away.
Quick tips for clinicians
Use controlled reperfusion, consider cooling, monitor biomarkers, and record arrhythmias. Combine mechanical and drug strategies when possible.
What patients should ask
Ask about risks, protective steps, signs to report, and follow-up plans. Bring a list of meds and allergies. Stay curious; second opinions can add valuable perspective anytime, too.