SGA Monitoring: What It Is, Why It Matters, and How It’s Done
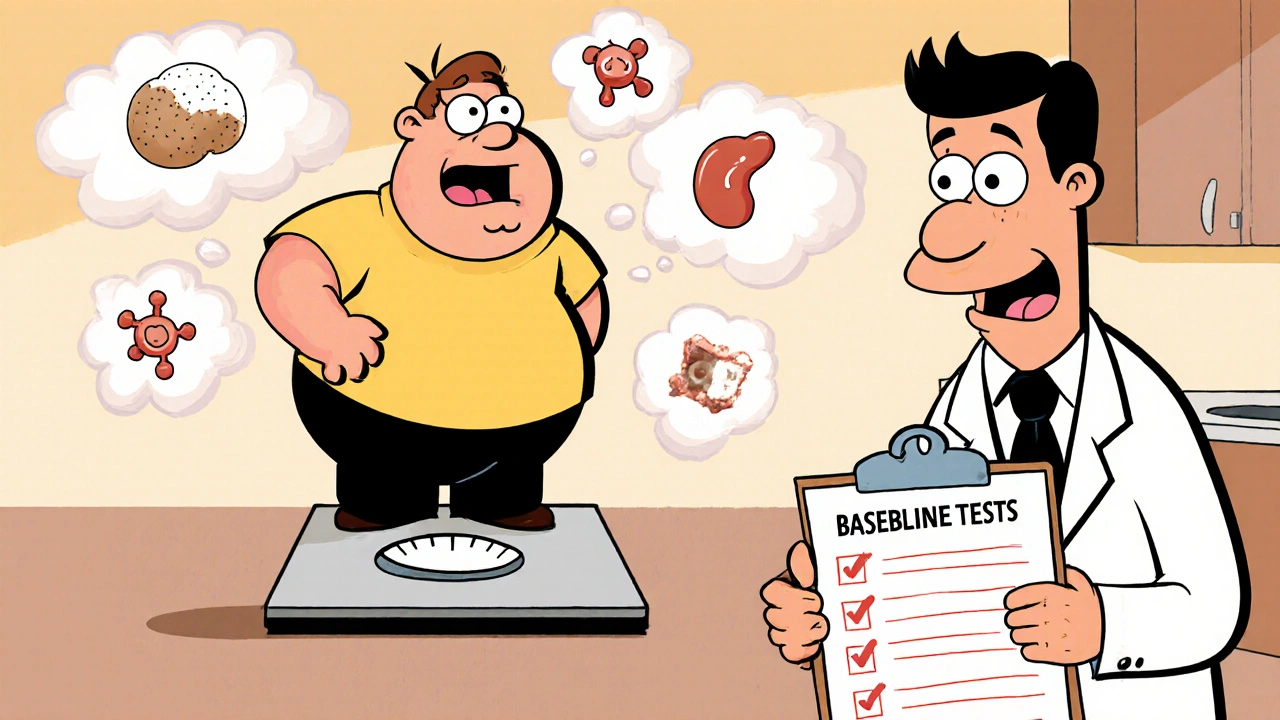
When someone takes a second-generation antipsychotic, a class of psychiatric medications used to treat schizophrenia, bipolar disorder, and other conditions. Also known as atypical antipsychotics, it SGA is designed to reduce psychotic symptoms with fewer movement side effects than older drugs. But they come with their own hidden risks—weight gain, high blood sugar, and bad cholesterol—that can lead to heart disease or diabetes if left unchecked. That’s where SGA monitoring, a structured process of tracking health changes in patients taking these medications comes in.
SGA monitoring isn’t optional—it’s standard care. The American Psychiatric Association and the FDA both recommend regular checks for weight, blood pressure, glucose, and lipids within the first few months of starting an SGA and then at least yearly after that. Why? Because studies show up to 40% of patients gain 7% or more of their body weight in the first year, and nearly one in three develop metabolic syndrome. These aren’t rare side effects—they’re predictable, preventable, and often missed because no one’s looking. Monitoring turns guesswork into action. It’s not just about catching problems early; it’s about giving patients a real shot at staying healthy while managing their mental illness.
What gets tracked? Weight and BMI are checked every month for the first three months, then every three to six months after. Fasting blood sugar and HbA1c tests catch rising glucose levels before diabetes sets in. Lipid panels check for triglycerides and LDL cholesterol spikes. Blood pressure gets measured at every visit—some SGAs raise it significantly. And if a patient’s numbers start climbing, doctors can switch meds, add metformin, or refer them to nutrition and exercise support. It’s not about stopping treatment—it’s about making it safer. The same principles apply whether someone’s on risperidone, olanzapine, quetiapine, or clozapine. Each SGA carries different risks, but all need monitoring.
Patients often don’t realize these changes are linked to their meds. They think gaining weight is just life, or that feeling tired is normal. But when you connect the dots—weight gain, high sugar, high cholesterol—it’s clear these aren’t random. They’re side effects. And they’re preventable with the right checks. That’s why SGA monitoring isn’t just a checklist. It’s a lifeline. The posts below cover real cases, practical tracking tools, how to talk to your doctor about these risks, and what to do when side effects show up. You’ll find guides on managing metabolic changes, comparing different SGAs, and understanding how long it takes for these effects to appear. This isn’t theoretical. It’s what keeps people alive and well on these drugs.