Tight Glycemic Control: What It Means and How It Affects Your Health
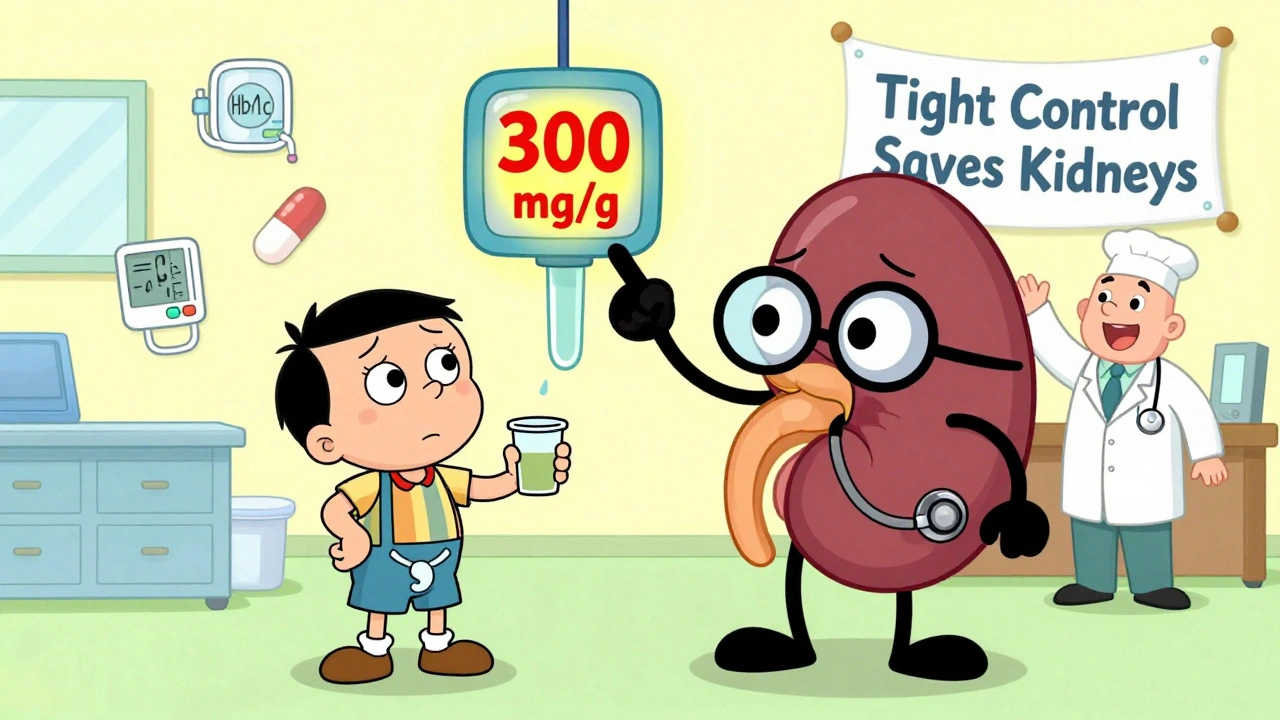
When doctors talk about tight glycemic control, the practice of keeping blood glucose levels as close to normal as safely possible to prevent long-term damage. It's not just about avoiding high numbers—it's about reducing the slow, silent harm that fluctuating sugars cause to your nerves, kidneys, eyes, and heart. This isn't a one-size-fits-all goal. For someone with type 1 diabetes, it might mean checking blood sugar six times a day and adjusting insulin with every meal. For someone with type 2, it could mean combining diet, movement, and medication to stay under 140 mg/dL after eating. The science is clear: keeping HbA1c below 7% lowers the risk of kidney failure, blindness, and amputations. But pushing too hard can lead to dangerous lows—so it’s a balance, not a race.
SGLT2 inhibitors, a class of diabetes drugs that help the kidneys flush out extra sugar through urine are one tool that makes tight control easier without causing hypoglycemia. Drugs like canagliflozin and dapagliflozin don’t just lower blood sugar—they also protect the heart and kidneys. But they come with trade-offs: higher risk of yeast infections and dehydration. That’s why monitoring and hydration matter just as much as the pill you take. And then there’s medication adherence, how consistently someone takes their prescribed drugs. No matter how good a drug is, if you miss doses, tight control falls apart. Studies show people who take their meds as directed cut their hospital visits by nearly half. Simple tools like pill organizers or weekly checklists can make a bigger difference than switching drugs.
Tight glycemic control isn’t just for people with diabetes. It’s also relevant for those with prediabetes, gestational diabetes, or even metabolic syndrome. Even if you’re not diabetic yet, keeping your sugars steady can delay or prevent the disease. It’s not about perfection—it’s about consistency. Small daily choices—like choosing water over soda, walking after dinner, or not skipping your metformin—add up. The posts below cover real-world strategies: how flavoring pediatric meds helps kids stay on track, why batch variability in generics can affect your results, how to avoid dangerous drug interactions, and what to do when insurance blocks your best option. You’ll find practical advice from people who’ve been there, not just theory from textbooks.