Transient Ischemic Attack (TIA)
When dealing with Transient Ischemic Attack, a short‑lived neurological event caused by temporary loss of blood flow to the brain. Also known as a mini‑stroke, it serves as a warning sign that a full‑blown stroke may be on the horizon. Most people experience symptoms that clear up within minutes, but the underlying problem often stays hidden. That’s why doctors treat a TIA as a red flag, not a harmless hiccup.
A stroke, a permanent interruption of cerebral blood supply leading to lasting brain damage can follow a TIA if the same blockage or clot persists. The relationship is straightforward: TIA predicts stroke, and early intervention can break that chain. Managing a TIA therefore requires a two‑pronged approach—control immediate symptoms and address the root causes that could trigger a future stroke.
One of the first steps in treatment is antiplatelet therapy, medication that reduces platelet aggregation to keep blood flowing smoothly. Drugs like aspirin or clopidogrel are commonly prescribed because they lower the chance that a small clot will grow and block a brain artery. While antiplatelet meds are powerful, they work best when paired with lifestyle changes that tackle high blood pressure, cholesterol, and diabetes—classic risk factors that fuel most TIAs.
Key Points About TIA
Understanding a TIA means looking at the bigger picture of vascular health. Carotid artery disease, plaque buildup that narrows the main vessels supplying the brain often lies at the heart of the problem. When the carotid arteries are narrowed, tiny clots can break off and briefly obstruct smaller brain vessels, creating the fleeting symptoms of a TIA. Imaging tests such as carotid ultrasound or CTA can confirm the degree of narrowing and guide whether a patient needs medication, lifestyle tweaks, or even a surgical procedure like carotid endarterectomy.
Besides the arteries, blood pressure is a silent driver. Even modest elevations can stress vessel walls, promote plaque rupture, and make clots more likely. That's why doctors ask patients to track their numbers at home and aim for a target below 130/80 mmHg in most cases. Coupled with a heart‑healthy diet, regular exercise, and smoking cessation, blood pressure control dramatically cuts the odds of a repeat TIA or a full stroke.
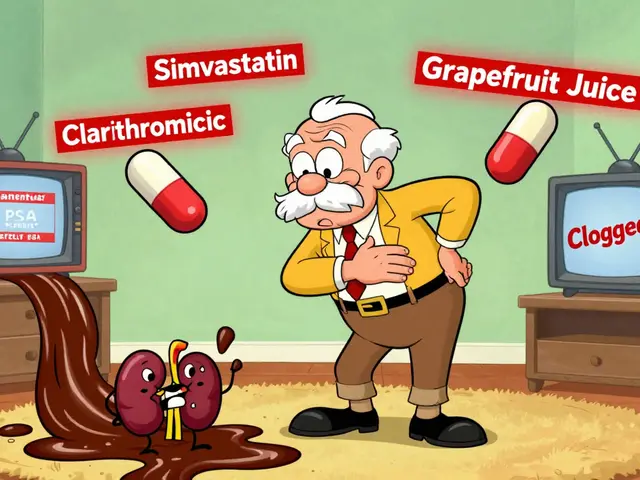
Another piece of the puzzle is cholesterol. LDL particles carry the building blocks of plaque, and high levels accelerate narrowing. Statins are the go‑to medication for most TIA patients because they not only lower LDL but also stabilize existing plaque, making it less likely to break apart. For younger patients with a family history of early strokes, genetic testing might reveal conditions like familial hypercholesterolemia, prompting even earlier and more aggressive therapy.
Timing matters, too. The risk of a stroke is highest within the first 48 hours after a TIA, then gradually tapers off. This short window is why emergency departments run fast‑track protocols: quick brain imaging, blood work, and a start on antiplatelet therapy can shave weeks off a patient’s recovery timeline and, more importantly, prevent permanent disability.
Finally, patient education rounds out care. People who recognize the classic TIA signs—sudden weakness, speech slur, vision loss, or balance trouble—are more likely to seek help fast. Teaching families the FAST acronym (Face drooping, Arm weakness, Speech difficulty, Time to call 911) turns a vague warning into actionable knowledge.
All these pieces—antiplatelet meds, blood pressure control, cholesterol management, carotid assessment, and rapid response—fit together like a checklist that keeps the brain safe. Below you’ll find a curated set of articles that dive deeper into each of these topics, offering practical tips, medication comparisons, lifestyle guides, and the latest research that can help you or a loved one navigate the world after a TIA.