When two or more drugs are combined into a single pill or formulation, the goal is simple: better results with fewer pills. But behind that simplicity lies a complex balancing act-especially when different doses or brands are swapped out. Therapeutic equivalence isn’t just a regulatory term; it’s the invisible rulebook that tells pharmacists and doctors whether one combination product can safely replace another without risking patient outcomes. For millions taking drugs like amlodipine/benazepril for high blood pressure or ezetimibe/simvastatin for cholesterol, getting this right means the difference between stable health and a hospital visit.
What Does Therapeutic Equivalence Actually Mean?
Therapeutic equivalence means two drug products have the same active ingredients, in the same amounts, delivered the same way, and produce the same clinical effect. The FDA’s Orange Book is the official source that rates these products. If a combination drug gets an ‘A’ rating, it’s considered interchangeable with the brand-name version. That’s why generic versions of Advair Diskus (fluticasone/salmeterol) can be sold for 40% less-because they’ve passed the same tests for absorption, strength, and performance. But here’s the catch: therapeutic equivalence doesn’t mean identical in every way. Two generic versions of the same combination product can have different fillers, coatings, or disintegrants. For most people, that doesn’t matter. But for drugs with a narrow therapeutic index-like warfarin, levothyroxine, or phenytoin-even tiny differences in how the body absorbs the drug can tip the balance from safe to dangerous.Why Dose Equivalence Gets Tricky in Combinations
A combination product isn’t just the sum of its parts. Sometimes, the drugs work together in ways that aren’t linear. Take tramadol and acetaminophen. Individually, each reduces pain. Together, they boost each other’s effect in a way that’s more than just adding 50mg + 325mg. That’s called synergy. But when you switch from one brand to another, or change the dose ratio, that synergy can break. Calculating dose equivalence for combinations isn’t like swapping one pill for another. It requires models like the one used in the Tallarida formula, which accounts for how much more effective one drug is than another. For example, if one drug in the combo is 88.9% effective at reducing cell growth and the other is only 69.8%, you can’t just match milligrams-you have to match biological impact. That’s why some generic versions of combination products, even with the same labeled doses, can still cause unexpected results.The FDA’s Rating System: A, B, and What It Really Means
The Orange Book uses a simple letter system, but the meaning behind it is anything but simple. An ‘A’ rating means the product is therapeutically equivalent. A ‘B’ rating means there’s uncertainty-usually because bioequivalence hasn’t been fully proven. This matters most with combination products that use the 505(b)(2) approval path, which allows manufacturers to rely on existing data but make changes to formulation or delivery. For example, a generic version of a combination product might use a different salt form of the active ingredient, or a new coating that changes how fast the drug is released. If those changes affect absorption, the FDA may assign a ‘B’ rating-even if the labeled doses are identical. That means pharmacists can’t automatically substitute it without checking with the prescriber.
Real-World Problems: When Equivalence Fails
A 2018 study in the Journal of Clinical Endocrinology & Metabolism found that 12% of patients switching between different levothyroxine generics had changes in their thyroid hormone levels-even though all products met FDA bioequivalence standards. That’s because the inactive ingredients affected how the thyroid hormone was absorbed in the gut. For patients on combination drugs like levothyroxine with a beta-blocker, even a small shift can cause fatigue, palpitations, or worse. Pharmacists on Reddit and Allnurses report similar stories. One pharmacist described three dosing errors in six months just from switching between different strengths of amlodipine/benazepril combinations. Another nurse practitioner saw a patient’s LDL cholesterol jump 15% after switching from brand-name Vytorin to a generic. The active ingredients were the same. The doses were identical. But the formulation was different-and so was the outcome. The FDA’s Adverse Event Reporting System logged 247 incidents in 2022 related to dose conversion errors in combination products. Nearly 40% involved cardiovascular drugs. Another 30% involved psychiatric combinations, where even minor fluctuations can trigger relapse or side effects.How to Manage Combination Products Safely
There’s no single fix, but there are proven steps that reduce risk:- Check the Orange Book-Always verify the TE code before substituting. Don’t assume ‘A’ means ‘safe to swap’ without context.
- Know the NTI drugs-If the combination includes warfarin, levothyroxine, phenytoin, or digoxin, treat it like a landmine. Avoid switching unless absolutely necessary, and monitor closely if you do.
- Use barcode scanning-Many hospitals now require scanning every combination product at the point of dispensing. This catches mismatches in strength or manufacturer before they reach the patient.
- Keep a 72-hour watch-After switching any combination product, especially for NTI drugs, check lab values, symptoms, and patient reports. Don’t wait for the next scheduled visit.
- Train your team-The University of California Health System cut substitution errors by 65% after a 40-hour training program for pharmacists and nurses. Knowledge is the best safeguard.
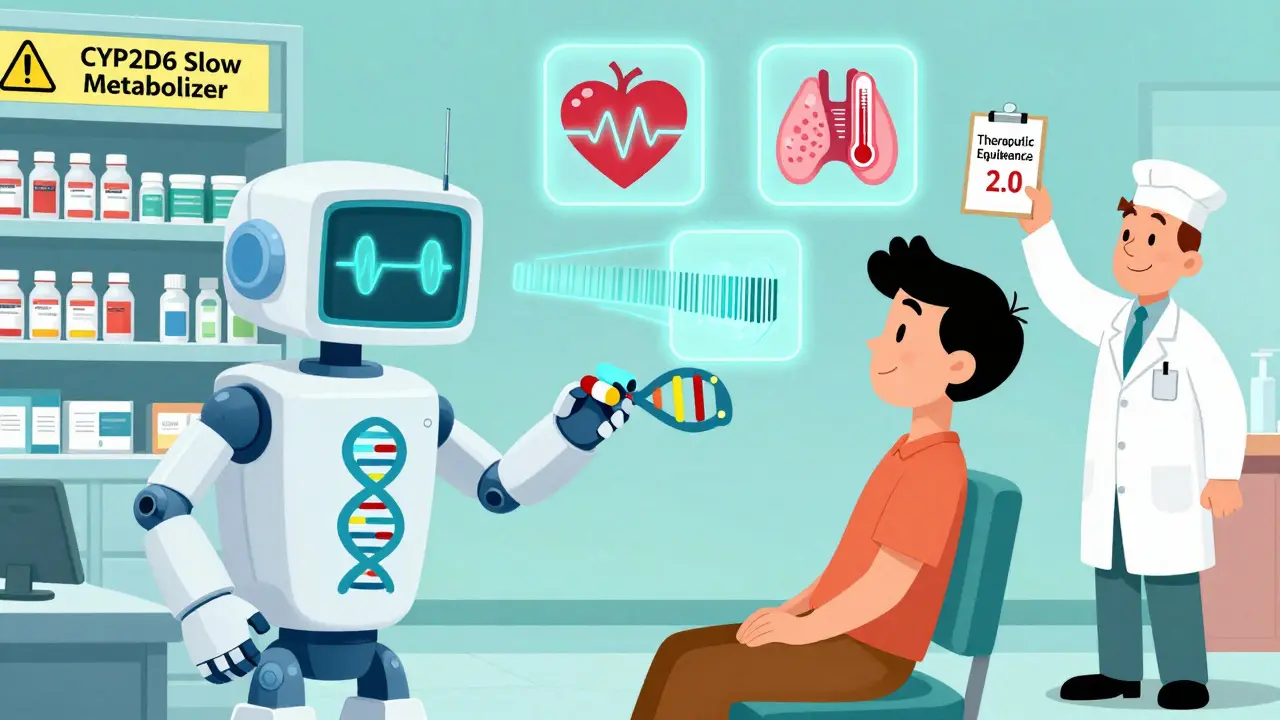
The Future: Personalized Equivalence?
The FDA is working on new tools to predict when a combination product might fail-even if it’s rated ‘A’. Early machine learning models have been 89% accurate at spotting problematic substitutions based on formulation differences. That’s a big step forward. But the real shift is coming from personalized medicine. By 2030, the NIH predicts that 30% of therapeutic equivalence decisions will include pharmacogenomic data. For example, if a patient metabolizes drugs slowly due to a CYP2D6 gene variant, a standard ‘A’-rated combination might still be too strong. Future systems may flag these patients automatically, suggesting a different formulation or dose adjustment before the prescription is filled. For now, the system works well for most people. But when it comes to combination products, especially those with narrow margins, therapeutic equivalence isn’t a finish line-it’s a starting point for careful monitoring.What You Need to Remember
- Therapeutic equivalence doesn’t mean identical in every way-just clinically equivalent. - Different inactive ingredients can still affect absorption, especially in NTI drugs. - Synergy in combination products makes simple dose matching unreliable. - Always check the Orange Book, and never assume a generic is automatically interchangeable. - Monitor patients closely after switching any combination product, especially those with heart, thyroid, or psychiatric conditions.Frequently Asked Questions
Can I switch between generic combination products without asking my doctor?
It depends. If the combination is rated ‘A’ in the FDA’s Orange Book and doesn’t contain a narrow therapeutic index drug, switching is usually safe. But if it includes warfarin, levothyroxine, phenytoin, or any psychiatric combo, always check with your prescriber first. Even ‘A’-rated generics can behave differently in some people.
Why do some generic combination products cost less but still get an ‘A’ rating?
Because they meet the FDA’s standards for bioequivalence and performance. The lower cost comes from reduced marketing, no patent fees, and lower R&D expenses-not from cutting corners on active ingredients. The ‘A’ rating means the drug performs the same way in the body, even if the pill looks different or contains different fillers.
What’s the difference between a pharmaceutical equivalent and a therapeutic equivalent?
A pharmaceutical equivalent has the same active ingredients, strength, dosage form, and route-but may differ in inactive ingredients. A therapeutic equivalent is a pharmaceutical equivalent that has been proven to produce the same clinical effect and safety profile. All therapeutic equivalents are pharmaceutical equivalents, but not all pharmaceutical equivalents are therapeutic equivalents.
Are combination biologics covered by therapeutic equivalence rules?
Not really. As of 2023, the FDA has only established therapeutic equivalence frameworks for 3 out of 47 approved combination biologic products. Biologics are too complex-made from living cells, not chemicals-to be judged by the same standards as small-molecule drugs. Biosimilars for these products are evaluated differently, and substitution is rarely automatic.
How can I find the TE code for a combination drug?
Go to the FDA’s Orange Book website and search by the brand name or active ingredients. The TE code will appear next to each product listing. For example, amlodipine/benazepril 5/20mg might show as ‘A01’. If the code starts with ‘B’, it means the FDA hasn’t confirmed therapeutic equivalence yet-don’t substitute without consulting a pharmacist or prescriber.