Diabetic Kidney Disease: Causes, Signs, and How Medications Affect It
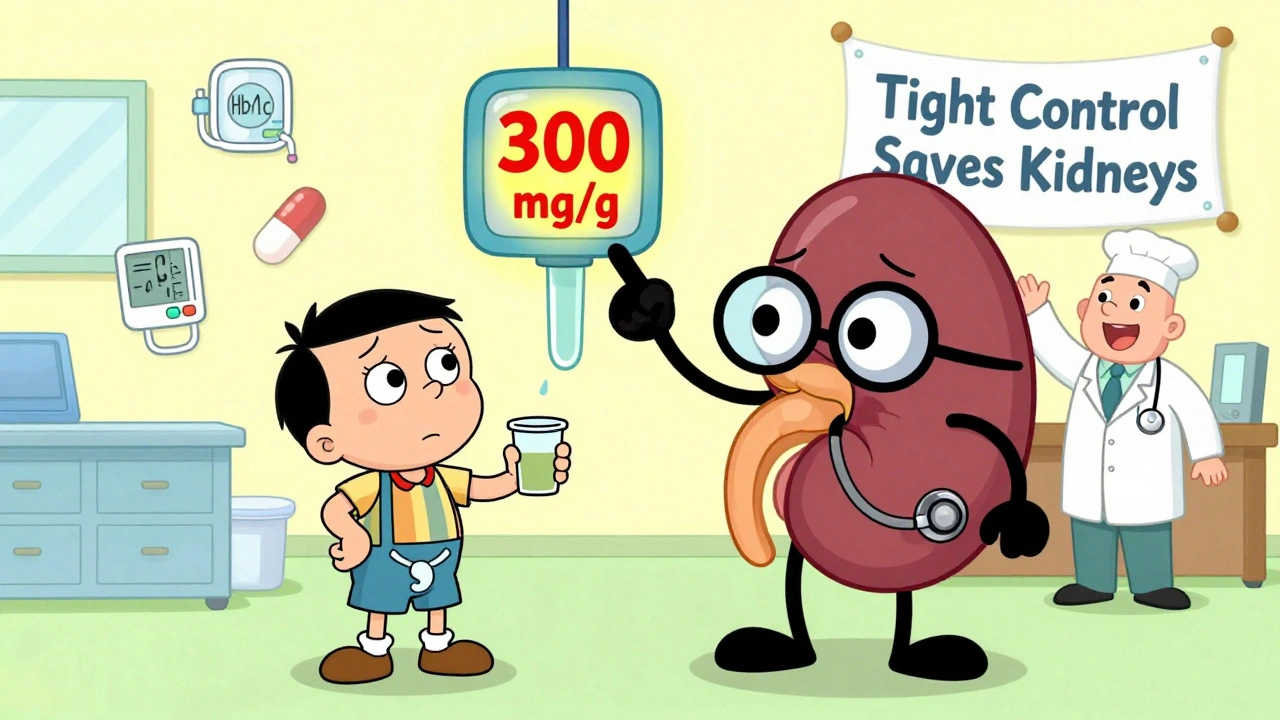
When you have diabetes, your body struggles to manage blood sugar—and over time, that stress can quietly damage your diabetic kidney disease, a progressive condition where high blood sugar harms the kidneys' ability to filter waste. Also known as diabetic nephropathy, it’s one of the leading causes of kidney failure in adults. This isn’t just about sugar—it’s about how that sugar interacts with tiny blood vessels in your kidneys, forcing them to work too hard until they start leaking protein and losing function.
Many people don’t feel symptoms until the damage is advanced. That’s why regular urine and blood tests are critical. Early signs include swelling in the feet, foamy urine, or rising blood pressure. The SGLT2 inhibitors, a class of diabetes drugs like canagliflozin and dapagliflozin have changed the game—they don’t just lower blood sugar, they actually slow kidney decline and reduce heart risks. But they can also raise the chance of yeast infections or dehydration, so monitoring matters. On the flip side, some common painkillers like ibuprofen or naproxen can make kidney damage worse, especially if you’re already at risk.
Managing chronic kidney disease, the broader term for long-term kidney function loss when it’s tied to diabetes means more than just taking pills. It’s about controlling blood pressure, cutting back on salt, staying hydrated, and avoiding drugs that strain the kidneys. The good news? Catching it early gives you a real shot at slowing or even stopping the damage. The posts below cover exactly how different medications—like SGLT2 inhibitors, statins, or even common antibiotics—interact with kidney health. You’ll find practical advice on tracking symptoms, understanding test results, and making smarter choices with your prescriptions. No fluff. Just what you need to protect your kidneys while managing diabetes.