Diuretics: What They Are and Why They Matter
When working with diuretics, medications that boost urine production to reduce excess fluid in the body. Also known as water pills, they help lower blood pressure, relieve edema, and correct fluid overload. In simple terms, diuretics encompass several sub‑categories, each targeting a different part of the kidney’s reabsorption process. Diuretics require prescription monitoring because the kidneys respond differently depending on the drug class. Excess sodium in the diet influences diuretic effectiveness, so lifestyle ties directly into how well the treatment works. This relationship between medication and diet forms a core part of managing conditions like hypertension and heart failure.
Key Types of Diuretics
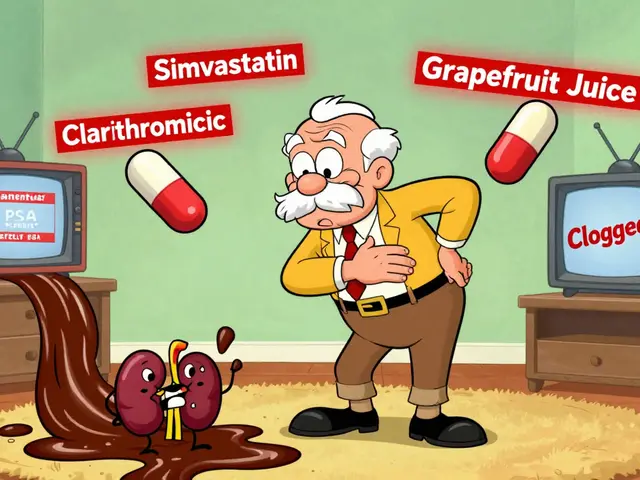
One major branch is loop diuretics, potent agents that act on the ascending limb of the loop of Henle. Common examples include furosemide and bumetanide, and they are prized for quickly removing large volumes of fluid, making them ideal for acute edema and severe hypertension. Another important group is thiazide diuretics, drugs that work in the distal convoluted tubule to moderate water and sodium loss. Hydrochlorothiazide and chlorthalidone fall here, offering a balance of blood‑pressure control with a lower risk of drastic fluid shifts. Finally, potassium‑sparing diuretics, agents that block aldosterone or sodium channels to retain potassium while still promoting urine output – spironolactone and amiloride are typical choices. Each class carries distinct attributes: potency, site of action, and impact on electrolytes, especially potassium. Knowing these values lets doctors match the right drug to a patient’s specific needs, whether it’s managing chronic hypertension, preventing heart‑failure‑related swelling, or protecting against low potassium levels.
Because diuretics change how the body handles electrolytes, regular lab checks are a must. Low potassium can cause muscle cramps, irregular heartbeat, and fatigue, while high potassium may also be dangerous. Adjusting diet, adding supplements, or picking a potassium‑sparing option can keep levels in the safe zone. Side effects like increased urination, dizziness, or dehydration are common, but most patients tolerate the medication well when dosing is individualized. In the collection below you’ll find detailed looks at medication tolerance, hormone interactions, and complementary therapies that often intersect with diuretic use. Whether you’re curious about how a specific drug works, want tips for minimizing side effects, or need a broader view of fluid‑balance management, the articles ahead give practical insights you can apply right away.