Pharmacovigilance: Understanding Drug Safety Monitoring and Real-World Side Effects
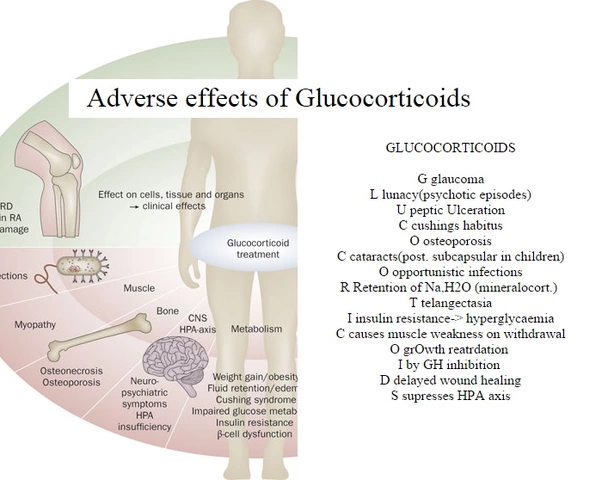
When you take a pill, you trust it will help—not hurt. That trust isn’t accidental. It’s built by pharmacovigilance, the science and activities focused on detecting, assessing, understanding, and preventing adverse effects or any other drug-related problems. Also known as drug safety monitoring, it’s the quiet system working behind every prescription, over-the-counter med, and supplement you use. This isn’t just lab data or clinical trial reports. It’s real people reporting headaches, rashes, dizziness, or worse after taking a drug. Those reports? They get collected, analyzed, and acted on—sometimes leading to black box warnings, dosage changes, or even drug withdrawals.
Pharmacovigilance doesn’t stop when a drug hits the market. In fact, that’s when it really kicks in. Clinical trials involve thousands, but real-world use involves millions. That’s where rare side effects show up—like a sudden drop in white blood cells after taking a new antibiotic, or unexplained fatigue linked to a cholesterol drug. That’s why posts on ezetimibe, a cholesterol-lowering medication often used alongside statins talk about stomach upset or muscle pain. Those aren’t just random complaints. They’re data points feeding into pharmacovigilance databases. Same with modafinil, a wakefulness-promoting agent used off-label for focus. When people report anxiety or insomnia, those aren’t just forum rants—they’re part of a global safety net.
It’s also why you’ll see posts about tazarotene, a topical retinoid used for acne and psoriasis and its skin-peeling side effects. Those aren’t just "normal" reactions. They’re tracked to see if the rate increases over time, or if certain groups—like older adults or people with sensitive skin—are more affected. Pharmacovigilance connects the dots between a drug’s intended use and its messy, unpredictable reality. It’s the reason your doctor asks, "Have you noticed anything unusual since starting this?"—because your answer could help someone else down the line.
This system doesn’t just protect patients—it shapes how drugs are used. When reports pile up about heat-related illness in people taking diuretics, medications that help the body get rid of excess fluid, guidelines change. Warnings get added. Doctors get alerts. That’s pharmacovigilance in action. It turns individual experiences into collective knowledge.
What you’ll find below isn’t just a list of articles. It’s a map of how real people interact with medications—and how those interactions shape safety standards. From how lurasidone, an antipsychotic used for schizophrenia and bipolar depression affects weight over months, to why wellbutrin, an antidepressant with a different mechanism than SSRIs might cause seizures in rare cases, these posts show the human side of drug safety. You’re not just reading about side effects. You’re seeing how those side effects become part of a larger story—one that keeps future patients safer.